Complex post-traumatic stress disorder (C-PTSD) and borderline personality disorder (BPD) are two mental health conditions that share some common symptoms, such as feelings of anxiety, depression, anger, and emptiness. Both conditions are linked to trauma, although the role of traumatic experiences in BPD is less certain compared to C-PTSD.
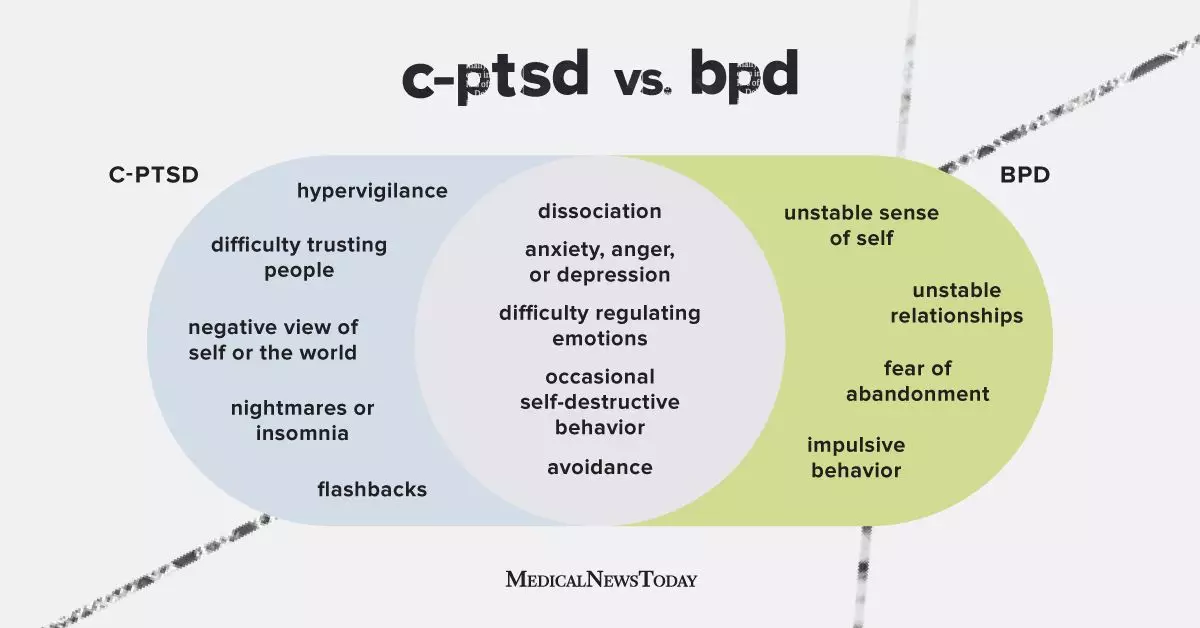
C-PTSD typically occurs in individuals who have experienced multiple or ongoing traumatic events, leading to a chronic sense of trauma that disrupts their ability to feel safe. Symptoms may include nightmares, flashbacks, difficulty trusting others, negative self-image, and emotional regulation issues. On the other hand, BPD is characterized by unstable relationships, emotional dysregulation, an unstable sense of self, and extreme relationship behaviors.
While both C-PTSD and BPD can develop following traumatic experiences and may share some overlapping symptoms, they are distinct conditions with unique characteristics. Individuals with C-PTSD tend to have a more stable but negative self-view, whereas those with BPD experience a fluctuating sense of self and often struggle with extreme relationships. BPD is a long-term condition that affects various aspects of an individual’s thinking and behavior, while C-PTSD may not necessarily impact every aspect of a person’s life.
It is possible for individuals to have both C-PTSD and BPD, as there is a significant overlap between the symptoms of these two conditions. In fact, research has shown that a substantial number of adults with BPD have also experienced post-traumatic stress disorder (PTSD) at some point in their lives. This overlap has led some experts to suggest that PTSD, C-PTSD, and BPD may exist on a continuum of post-traumatic stress disorders.
Doctors may sometimes misdiagnose C-PTSD as BPD or vice versa due to various reasons, including symptom overlap, lack of awareness of C-PTSD as a separate condition, gaps in memory related to trauma, comorbidity with other mental health conditions, and complex diagnostic criteria. A comprehensive evaluation by a mental health professional is essential for accurately diagnosing C-PTSD and BPD, which may involve clinical interviews, assessments, consideration of coexisting conditions, and input from family members or caregivers.
Treatment for both C-PTSD and BPD typically involves a multifaceted approach that may include therapy and medication. Trauma-focused therapy is the primary treatment for C-PTSD, helping individuals process traumatic memories and improve their daily functioning. Various types of talk therapy, such as dialectical behavior therapy (DBT), are commonly used to treat BPD, aiming to help individuals better understand their emotions, develop healthier relationships, and manage impulsive behaviors.
While there are no medications that specifically cure C-PTSD or BPD, medications may be prescribed to manage associated symptoms, such as anxiety or mood shifts. Individuals with both C-PTSD and BPD may benefit from a combination of trauma therapy, psychotherapy, and medication to address the underlying causes and improve long-term symptom management.
It is essential for individuals experiencing persistent emotional distress, overwhelming sadness, anxiety, or thoughts of self-harm to seek help from a mental health professional. Support and treatment are available for those with C-PTSD and BPD, with various therapy options designed to alleviate symptoms and improve mental well-being. Seeking early intervention and support can make a significant difference in managing these complex mental health conditions.