Blood donation is an essential practice that saves countless lives. However, many donors may not be aware of the intricate testing and criteria involved in ensuring the safety and efficacy of the donated blood. Although all collected blood undergoes routine testing to identify specific conditions and factors, not all potential health issues, such as leukemia, are screened for during the donation process. Despite this, abnormalities can sometimes surface, prompting further investigation into the donor’s health.
The preliminary assessment that each blood donor undergoes is a critical step in the donation process. This procedure, commonly referred to as a mini health assessment, evaluates vital signs such as pulse, blood pressure, temperature, and hemoglobin levels. Hemoglobin is crucial as it carries oxygen throughout the body. If these levels are found to be outside the normal range, it may raise red flags. Low hemoglobin can indicate various health problems, including anemia or even conditions like leukemia. Therefore, donors with significant blood abnormalities are typically advised against donating.
Blood Testing and Its Limitations
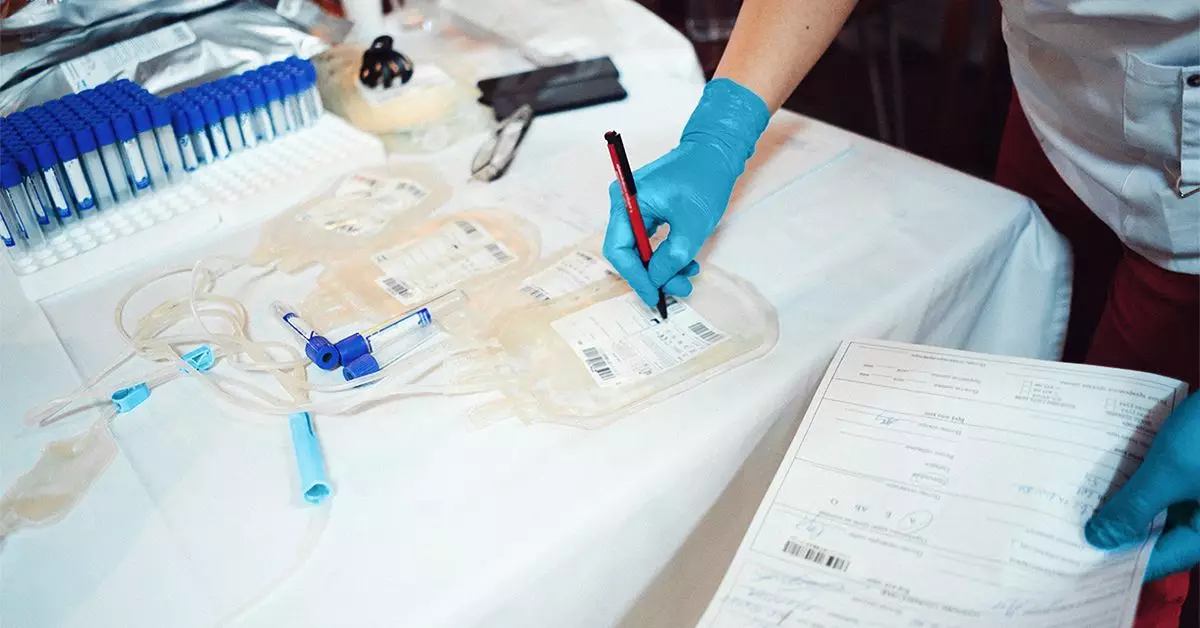
Once blood is collected, it enters a meticulous screening and processing phase to ensure its safety for transfusion. Organizations like the American Red Cross utilize rigorous screening methods to test blood for type, infectious diseases such as HIV, hepatitis, and syphilis, as well as sickle cell traits. However, there remains a notable limitation in that testing does not routinely include checks specifically for leukemia.
Interestingly, certain infections, like HTLV-1, can increase the risk of adult T-cell leukemia, demonstrating a rare, indirect connection between infectious disease and leukemia risk. When a blood test suggests a positive result for such infections, the donation is immediately discarded, and the donor is usually notified.
Yet, an alarming aspect of this system is its tendency to overlook the potential for underlying conditions that remain undiscovered until a person’s blood is tested. If abnormalities are identified during processing, blood donation centers may reach out to the donor, advising them to seek further medical evaluation. This potential for an undiagnosed condition highlights a critical intersection between blood donation and the importance of proactive health monitoring.
Making Informed Health Choices
Being aware of blood health is crucial for both donors and the healthcare system. Individuals with a history of leukemia or related conditions are outright prohibited from donating blood. Furthermore, as awareness grows about the various underlying health issues that can manifest during the blood donation process, it prompts an essential conversation about the importance of regular health check-ups beyond the scope of blood donation.
While the blood donation process is invaluable to saving lives, it is rife with complexities that merit serious consideration. Donors need to understand not only the procedure but also the potential health implications that may arise from their participation. Staying informed and engaged with personal health can lead to better outcomes for both donors and recipients, reinforcing the vital link between blood donation and overall health vigilance.