Cancer treatment is an essential aspect of fighting the disease, but it can also have significant repercussions on the body. Radiotherapy, chemotherapy, and surgery are common forms of cancer treatment that can inadvertently damage the thyroid gland. The thyroid plays a crucial role in regulating energy use in the body by producing essential hormones. However, when cancer treatments interfere with the thyroid’s function, it can lead to the development of hypothyroidism, an underactive thyroid condition.
Effects of Cancer Treatments on the Thyroid
Various cancer treatments can impact thyroid health in different ways. For example, surgery or radiation therapy may directly damage or remove thyroid tissue, impairing its ability to produce essential hormones. Moreover, some chemotherapy drugs or medications can block thyroid hormone production or trigger an immune response against the thyroid gland. In some cases, treating certain types of cancer can elevate the risk of hypothyroidism regardless of the specific treatment method used. Research has shown that individuals who have undergone treatment for breast cancer are at a higher risk of developing hypothyroidism, with combined chemotherapy and radiation therapy posing the greatest risk.
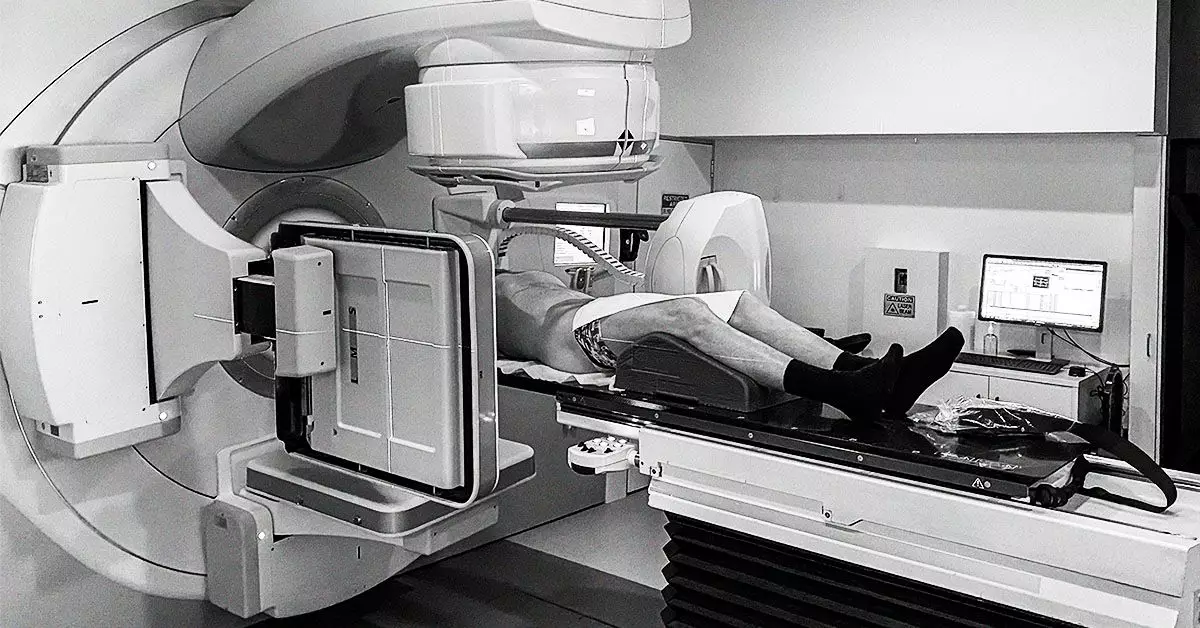
Radiation Therapy and Hypothyroidism
Radiation therapy, particularly in the treatment of head and neck cancers, poses a significant risk of hypothyroidism. Studies have indicated that as many as 40 to 50% of individuals who receive radiation therapy may develop hypothyroidism. The thyroid gland is especially susceptible to radiation, leading to the destruction of thyroid tissue and a subsequent decline in thyroid hormone production. Factors influencing the risk of hypothyroidism following radiation therapy include the radiation dose, the type of radiation therapy received, the size of the thyroid gland, and the individual’s age and sex.
Surgery to remove thyroid tissue containing cancer cells is a common treatment for thyroid cancer. However, this can result in the destruction of thyroid cells, leading to hypothyroidism as the gland’s ability to produce thyroid hormone is compromised. Hormone therapy medications may also block the production of thyroid-stimulating hormone (TSH), which is essential for thyroid hormone synthesis. While hormone therapy may reduce the risk of thyroid cancer recurrence, it can also induce hypothyroidism.
Immunotherapy and Hypothyroidism
Immunotherapy, which involves using drugs to target cancer cells through the immune system, can also impact thyroid function. In particular, immune checkpoint inhibitors may lead to thyroid inflammation as the immune system targets thyroid tissue. Although this inflammation may precede the development of hypothyroidism, individuals who experienced thyroid issues during immunotherapy had higher cancer survival rates.
Individuals who develop hypothyroidism as a result of cancer treatment may need to undergo thyroid hormone therapy for the rest of their lives. Levothyroxine, a synthetic form of thyroid hormone, is commonly prescribed to maintain energy metabolism in the body. By ensuring adequate thyroid hormone levels, the risk of thyroid cancer recurrence may be reduced. Moreover, certain types of cancer, such as pituitary gland tumors and papillary thyroid cancer, may also be associated with the development of hypothyroidism.
Cancer treatment can have profound effects on thyroid health, leading to the development of hypothyroidism. It is essential for healthcare providers to monitor thyroid function in individuals undergoing cancer treatment to promptly address any thyroid-related complications. By understanding the impact of cancer treatments on the thyroid, healthcare professionals can provide comprehensive care to cancer patients and improve treatment outcomes.